How do you increase quality in claims assessment, management and administration? We share insights into an end-to-end, AI-powered, claims-automation approach to increase quality, improve processing efficiency and reduce cost.
In this blog series, I’ve spoken about how AI increases process efficiency, reduces costs and helps business solve problems. I also showed how it enables smart business transformation by creating intelligent processes at every step along the value chain and intelligent products and services in the market. In my previous post, I illustrated how insurers can use AI-related technologies in underwriting and service management. Now, I’ll explain how AI helps insurers to manage claims more effectively and efficiently. How can insurers use AI in claims management? AI technologies make information systems more adaptive to humans and improve the interaction between humans and computer systems. By doing this, AI gives insurers an edge on how they manage claims—faster, better and with fewer errors. Insurers can achieve better claims management by using the intelligent technologies in some of the following ways:- To enable a real-time question-and-answer service for first notice of loss;
- To pre-assess claims and to automate damage evaluation;
- To enable automated claims fraud detection using enriched data analytics;
- To predict claim volume patterns;
- To augment loss analysis
 With our machine learning solution in place, a fully automated process was enabled and took only three minutes to do the same amount of work. This represents a 74% reduction in the claims settlement time.
Furthermore, the machine learning technology applied was able to process health claims with 80% accuracy. The other 20% are incorrectly processed owing to spelling errors or database limitations. However, machine learning technologies are able to store and recall those errors for more accurate claims processing in the future.
Case study 2: AI-powered automation of automobile claims processing
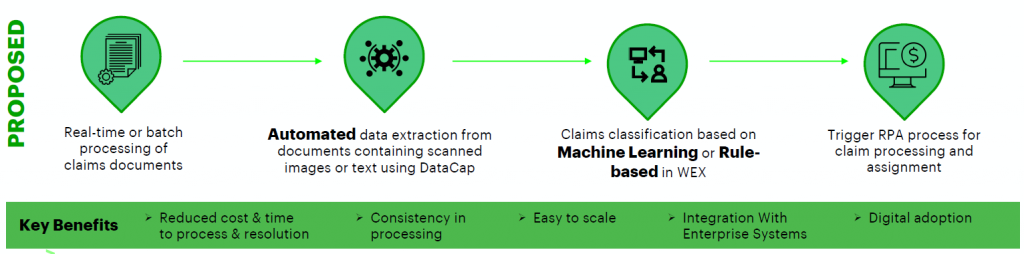
Accenture was recently part of a major client initiative to identify technologies and partner for an AI-driven automation journey. We proposed and built a solution to automate processes to extract and classify data from commercial automobile claims PDF documents.
The client faced many challenges, including having fewer than 400 records to classify 55 unique cases, and these records were mismatched and labeled inconsistently. The client also received scanned images containing text, owing to the redaction process followed to ensure data privacy.
We developed an on-premise solution using a combination of IBM offerings and open-source technologies that enabled a detailed analysis of training data. The solution also helped the client to identify quality and sparse/skew data and to test various approaches to maximize performance.
In the end, a blind data set of 207 claims documents was processed within a four-hour assessment window, and we were able to process claims PDF documents with scanned images as well as text, including several formats and layouts not part of training data.
See also: How to Use AI, Starting With Distribution
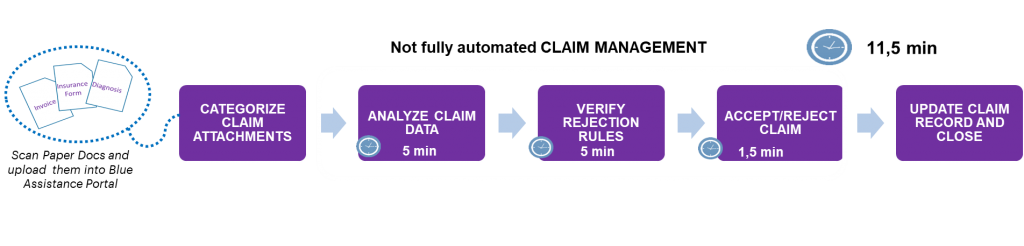
We identified several pain points in the current claims management process:
With our machine learning solution in place, a fully automated process was enabled and took only three minutes to do the same amount of work. This represents a 74% reduction in the claims settlement time.
Furthermore, the machine learning technology applied was able to process health claims with 80% accuracy. The other 20% are incorrectly processed owing to spelling errors or database limitations. However, machine learning technologies are able to store and recall those errors for more accurate claims processing in the future.
Case study 2: AI-powered automation of automobile claims processing
Accenture was recently part of a major client initiative to identify technologies and partner for an AI-driven automation journey. We proposed and built a solution to automate processes to extract and classify data from commercial automobile claims PDF documents.
The client faced many challenges, including having fewer than 400 records to classify 55 unique cases, and these records were mismatched and labeled inconsistently. The client also received scanned images containing text, owing to the redaction process followed to ensure data privacy.
We developed an on-premise solution using a combination of IBM offerings and open-source technologies that enabled a detailed analysis of training data. The solution also helped the client to identify quality and sparse/skew data and to test various approaches to maximize performance.
In the end, a blind data set of 207 claims documents was processed within a four-hour assessment window, and we were able to process claims PDF documents with scanned images as well as text, including several formats and layouts not part of training data.
See also: How to Use AI, Starting With Distribution
We identified several pain points in the current claims management process:
- Error-prone manual data extraction;
- Inconsistent claim classification;
- The need for additional downstream validation;
- Increased time and cost for processing and resolution.
 In the next post, I’ll look at how AI-related technology can be used to improve customer services and policy administration. Get in touch to find out how you can use AI in the entire insurance value chain, or download the How to boost your AIQ report.
In the next post, I’ll look at how AI-related technology can be used to improve customer services and policy administration. Get in touch to find out how you can use AI in the entire insurance value chain, or download the How to boost your AIQ report.